Novel Coronavirus SARS-CoV-2 This scanning electron microscope image shows SARS-CoV-2 (round magenta objects) emerging from the surface of cells cultured in the lab. SARS-CoV-2, also known as 2019-nCoV, is the virus that causes COVID-19. The virus shown was isolated from a patient in the U.S. NIAID-RMLCaption
As the number of confirmed COVID-19 cases increased in Asia and began to spread to other regions around the world, a team of employees at Gilead’s manufacturing site in La Verne, California met in the early morning of Monday, Feb. 3.
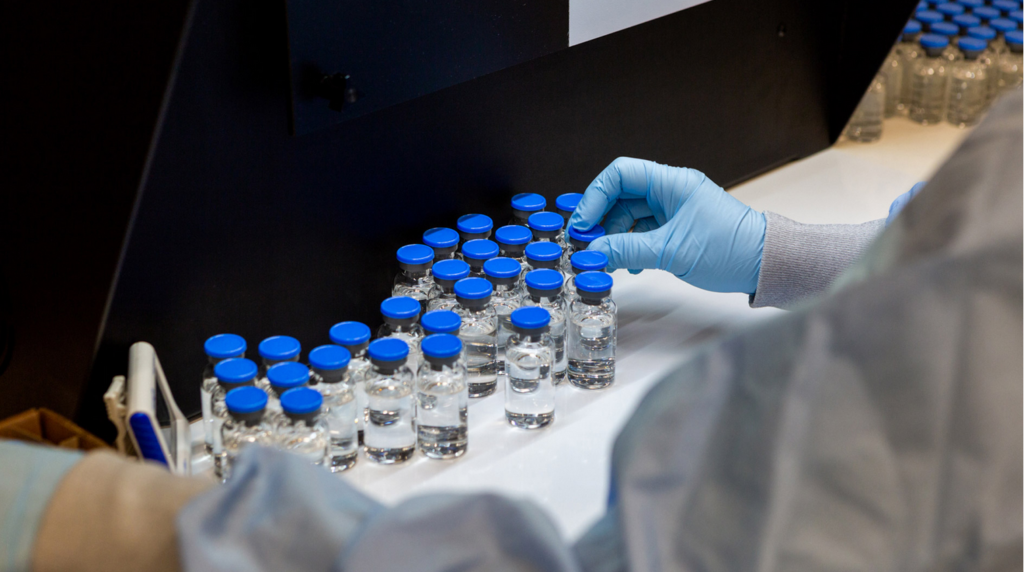
The topic of the meeting: How quickly could the site begin to formulate, fill, package and ship Gilead’s investigational COVID-19 treatment, remdesivir?
“From that moment on, it was all hands on deck,” says Charlie Langdon, Senior Director of Manufacturing in La Verne. “It wasn’t just one department – this was literally our entire site coming together and strategizing about what needed to be done to make this happen as quickly as possible.”
Just eight days later on Tuesday, Feb. 11, the La Verne site was filling its first vials of remdesivir to support clinical studies and emergency use protocols for patients in critical condition with few options. The team began a six-week campaign to fill up to 25,000 vials of the investigational COVID-19 treatment every other day, while at the same time packaging and shipping vials of the drug received from external manufacturing partners.
Remdesivir is an investigational drug that has not been approved by any regulatory authority, and the safety and efficacy of remdesivir for the treatment of COVID-19 are not yet known. However, the drug supply is urgently needed to support multiple ongoing clinical trials, as well as expanded access programs created in consultation with regulatory authorities worldwide.

Gilead opened the La Verne site in 2017 with state-of-the-art equipment and automation – which along with the team’s experience building out and running the facility was helpful in preparing the site to quickly pivot to remdesivir manufacturing, says Richard Aman, Senior Director of the Project Management Office in La Verne.

“The biggest thing was that we didn’t try to divide and conquer – instead we had every department involved in making the decisions,” says Richard. “Every single person at our site is playing a critical role in this effort.”
Still, there were challenges to overcome – new batch sizes of the drug product, new documentation requirements for the highly regulated process and a new manual inspection process that involves carefully inspecting each vial one-by-one.
“The most challenging part was getting started, but ever since we got up and running and did the first batch, we haven’t stopped,” says Huy Pham, Associate Director of Technical Services in La Verne.
To keep employees safe, the leadership team at La Verne has implemented physical distancing practices and worked to ensure that only people who need to be present to directly support manufacturing are on site.
Team members say they are inspired by the opportunity to play a role in potentially addressing this significant public health crisis.
“We all feel privileged and proud to be part of manufacturing this treatment that we hope can make a difference in the fight against COVID-19,” says Danielle Torres, Associate Director of Quality Assurance in La Verne. “With that also comes a great sense of responsibility, here in La Verne and at all levels of the organization. We can feel the potential magnitude of what we’re working on.” (Stories@Gilead)
An Open Letter from GILEAD’S Chairman & CEO
An update from our Chairman & CEO Daniel O’Day about clinical trials for our investigational treatment.
Earlier today, the New England Journal of Medicine (NEJM) published an analysis of the effects of our investigational medicine remdesivir on a small group of patients with severe symptoms of COVID-19.
These are patients who received treatment through the compassionate use program for remdesivir, which is for critically ill patients who are unable to take part in a clinical trial. The results, which cover 53 of the first patients to have been treated in the program, show that the majority demonstrated clinical improvement after taking remdesivir. We recognize the limitations of these compassionate use data from a purely investigational perspective, while knowing they are of the greatest significance for the patients whose symptoms improved. These early data from 53 patients have not been generated in a clinical trial and cover only a small portion of the critically ill patients who have been treated with remdesivir.
Remdesivir is an investigational treatment and has not been approved for use anywhere in the world. In the broader efforts to determine whether it is a safe and effective treatment, we have some way to go. Multiple clinical trials are underway across the world to build a complete picture of how remdesivir works in various contexts. These studies cover a range of patient populations across different demographics and with varying types of symptoms: moderate, severe where patients need oxygen support, and critical where medical ventilation is required. These patients all receive remdesivir through intravenous infusions in a hospital setting.
In studying remdesivir, the question is not just whether it is safe and effective against COVID-19 but in which patients it shows activity, how long should they receive treatment and at what stage of their disease would treatment be most beneficial. Many answers are needed, which is why we need multiple types of studies involving many types of patients.
Some of these answers will start to emerge in the coming weeks as we receive the first data from the various clinical trials underway.
Clinical trials for remdesivir
Seven clinical trials have been initiated to determine whether
remdesivir is a safe and effective treatment for COVID-19. Each of these
was set up with unprecedented speed thanks to the remarkable efforts of
the various groups involved, as well as the level of knowledge we had
on remdesivir.
To some extent, the trials have had to be adaptive in design as our understanding of the disease itself continues to evolve. The virus emerged and spread at an intense speed and everyone is working quickly to understand it. Our interpretation of the results will also be shaped by what we continue to learn about the disease.
The order in which the trials were initiated mirrors the path of the pandemic. China initiated the first two studies in early February for patients with severe and moderate symptoms of the disease. Since then, an additional five trials have been initiated around the world.
Two Phase 3 studies are being run by Gilead in areas with a high prevalence of COVID-19 in the United States, Asia and Europe. One of these is for patients with severe disease and the other studies remdesivir in patients with more moderate symptoms. One of the many questions that these studies aim to answer is whether treatment duration can be shortened from 10 days to 5 days. The severe arm fully enrolled the number of patients it was originally designed for and we have now expanded the study so that thousands more patients can participate, including those on mechanical ventilation.
The U.S National Institute of Allergy and Infectious Disease (NIAID) began a global trial on February 21. This trial randomly assigns patients to treatment with either remdesivir or with a placebo to enable a controlled comparison of outcomes. The trial is enrolling approximately 800 patients with a broad spectrum of symptoms.
The World Health Organization is also conducting a global trial, Solidarity, and the Inserm DisCoVeRy trial recently began in Europe. A summary of remdesivir trials with upcoming data readouts can be found here.
We know that there is tremendous interest around when the data from these trials will be available and what they will tell us about remdesivir. We feel the urgency as we wait for the science to speak. With every day that goes by, the desperate need to equip healthcare workers and their patients with a safe, effective treatment becomes more pressing. We are working with intense speed to determine whether remdesivir could be an option and we are committed to sharing information when it becomes available to us.
We expect that we will have preliminary data from the study of remdesivir in severe patients at the end of April and will work quickly to interpret and share the findings. The publication of data from the China remdesivir trials rests with the Chinese investigators, but we have been informed that the study in patients with severe symptoms was stopped due to stalled enrollment. We look forward to reviewing the published data when available. In May, we anticipate the initial data from the placebo-controlled NIAID trial as well as data from the Gilead study of patients with moderate symptoms of COVID-19.
To a large extent, the timelines are determined by epidemiology and the numerous challenges that come with studying a treatment for a newly emerged disease. As with so much in this pandemic, this is unchartered territory for many of us involved in the process.
Ongoing collaboration
While it may feel like a long wait for data given the urgency of the
situation, it has been only two months since the first clinical trials
began. Given that it can take a year or more to have the first clinical
data for an investigational treatment, it is remarkable that we expect
to have the first remdesivir trial data so soon.
This speed is the result of strong collaboration and immense dedication among the many groups involved, from regulatory authorities to hospital administrators, clinicians and study investigators. As with all the work on remdesivir, everyone is driven by the same sense of urgency and a commitment to maintaining scientific rigor throughout.
All of us at Gilead are grateful to the many groups and organizations who are collaborating to find answers on remdesivir and above all, to the physicians and patients involved in the clinical trials. When we talk about trial results, we tend to think in terms of numbers, trends and statistics. We realize that behind each of these numbers is a patient who has agreed to take part in a trial and share the data from their personal experience. It is thanks to the thousands of patients like these and the physicians who are treating them, that we will be able to determine whether remdesivir can be used safely and effectively for many more patients in the future.
Daniel O’Day – April 10, 2020
On May 1 the U.S. Food and Drug Administration Issued an Emergency Use Authorization for antiviral drug remdesivir for the treatment of suspected or laboratory-confirmed COVID-19 in adults and children hospitalized with severe disease.
Click here to read the 2020 May edition of Europe Diplomatic Magazine